May 4, 2011 — Oxford Health Plans, a UnitedHealthcare company, is rolling out renewal plans this spring for small businesses of two to 50 employees whereby the company is increasing the total employee financial responsibility for an out-of-network doctor visit or procedure by more than 50 percent.
In 2009, according to an Apr. 2011 report by the United Hospital Fund, 27.2 percent of small group health plan subscribers in the commercial market were enrolled in Oxford/United plans, a larger share than that of any other company.
According to notices of the changes applicable to at least some of Oxford’s “Freedom” Plans, Oxford is moving away from reimbursement for out-of-network care that is based initially on a percentile of “usual, customary, and reasonable charges” or “UCR.”
Under the new scheme, allowable charges are based on 140 percent of the Medicare reiumbursement rate, where such a rate is available.
Reimbursement ultimately winds up to be marginally less than Medicare, however, because — as demonstrated by the illustration Oxford gives in its notice — only 70 percent of that “Medicare plus” amount is reimbursed.
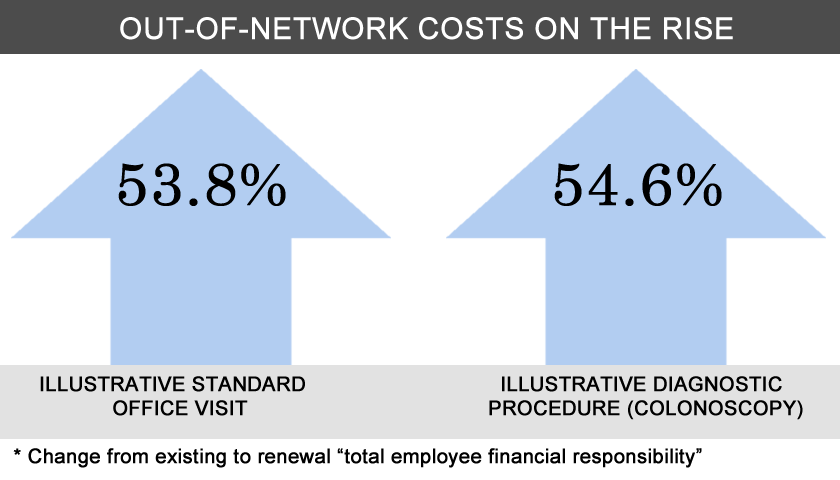
Significantly increased cost to the patient who chooses out-of-network care
Under an existing plan, Oxford says, an out-of-network colonoscopy would require a patient with Oxford insurance to pick up $2,180 in charges; under the revised payment schedule, the patient would be responsible for $3,370 in charges.
Oxford’s notice, which Remapping Debate received as part of its own health insurance renewal process, emphasizes the “cost effective” nature of in-network care, and makes plain its intention to have patients — no longer able as a practical matter to afford to see out-of-network providers — pressure those providers to join the Oxford network: “We believe that this change will encourage non-participating providers to join the network,” the notice stated.
New York State Assemblyman Richard N. Gottfried, the chair of the Assembly’s Health Committee, described Oxford’s push to shift people away from out-of-network care as “pretty heavy handed,” and said that the shift will have “several harmful consequences.”
“While Oxford [members] will technically have the choice of going out of network,” Gottfried said, “for many of them that will not be a realistic option, so it is, in effect, a dramatic restriction of their health care options.”
Mark Scherzer is a New York attorney whose practice includes representation of individuals challenging insurance company decisions denying benefits. He also acts as legislative counsel to New Yorkers for Accessible Health Coverage, which represents a series of groups of people with chronic illness or disability.
Scherzer said that Oxford’s reduction in reimbursement for out-of-network care was “consistent with the trend over the recent years…of trying to limit premium increases through other mechanisms [by] which costs are shifted to the consumer.”
Scherzer described the current system as one where insurance companies are “doing the rationing” of health care: “people with resources will get that high quality of [patient-centric] care, and people without resources won’t.”
Remapping Debate asked Oxford to confirm the reported changes, and to comment on the disjunction between its decision to cut out-of-network benefits sharply at the same time it was not cutting premiums: Wouldn’t these cutbacks save Oxford a lot of money over what had been paid out previously, and, if so, why wouldn’t premiums be going down?
Oxford’s email reply, from company representative Maria Gordon-Shydlo, was not responsive, and a follow-up request was not responded to.
According to Gottfried, the change “will help Oxford’s bottom line” but “will be bad news for patients and health care providers.”
An interesting way to count
The Oxford notice of benefit changes tried to provide assurance that patients could still be served in-network by a robust panel of doctors, stating that the network (as of the end of 2009) had “48,000 Freedom Network providers” in New York State. This number is not exactly what it seems at first glance. One must review a footnote to learn that the number doesn’t only refer to doctors, but also dentists and “complementary and alternative medicine providers.”
The footnote — which also made no mention of how many of those providers are currently accepting new patients — explained that each provider was being counted more than once if they had multiple board certifications (for example, primary care and a specialty).
Indeed, when Remapping Debate looked specifically for internists located within a mile of one physican-rich Upper East Side Manhattan zip code, the first 100 people yielded what Oxford would tally as 171 providers.
We asked Oxford why it counted the way it did, and asked for the actual number of in-network physicians in New York City and in New York State. Gordon-Shydlo said in an email that Oxford’s count was intended to convey the “depth and breadth” of the network — allowing enrollees to see a provider listed as both a primary care doctor and as a specialist — but she did not provide the requested information.
In a follow-up email, we reiterated our request for actual headcount, and asked: “If you wanted to reflect depth and breadth, couldn’t you say, ‘We have X physicians, Y percentage of whom are both primary care physicians and specialists or have two or more specialties’? Wouldn’t that give both pieces of [information]?”
Oxford did not respond.
Additional reporting by Mike Alberti and Althea Webber.