Warnings of doctor shortage go unheeded
Consequences for patient care
According to George Sheldon, the director of the Health Policy and Research Institute of the American College of Surgeons, as the physician-to-population ratio falls, current healthcare access issues will likely be exacerbated. Sheldon said that the shortage will be felt most acutely in rural communities, many of which already face healthcare access problems.
In metropolitan areas, where there is a greater concentration of doctors, the shortage will likely translate to longer wait times and a larger burden on individual doctors, and could also eventually lead to problems getting a appointments, added Richard Cooper, the former dean of the Medical College of Wisconsin who has long warned of the physician shortage.
Recent surveys of patients receiving care in urban areas show that appointment wait times have already increased in the last five years. Other reports show that the average length of a primary care appointment in 2009 was just 20 minutes, and that family physicians see nearly 17 patients per day, on average.
Christiane Mitchell, senior legislative analyst for the AAMC, also foresees these problems getting worse. “You’ll see a lot more people who can’t get access to care. You’ll see people who can’t get appointments, and you’ll see doctors having to take on more patients,” she said.
A long pipeline
Because patients will be showing up in record numbers just as doctors will be retiring in record numbers, it appears that minor boosts to physician supply would be wholly inadequate. According to a report issued by the AAMC, “even a moderate growth in supply requires substantial inflow to replace the substantial number of currently practicing physicians who will be leaving the workforce in the next 20 years.”
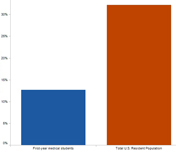
Med School Enrollment Versus Total Population
Map & Data Resources
Percent increase in first-year medical school enrollment and in U.S. population, 1983 to 2010.
To put the matter in context, U.S. medical schools only graduated 16,838 students in 2010, a relatively small increase compared with the 15,676 graduates in 2002, and a pittance in view of the coming demographic storm. (Indeed, the number of medical school graduates in the U.S. is not sufficient to fill the residency slots available, which meant that, in 2010, 20 percent of the applicants matched to first year residencies were educated abroad, according to the National Resident Matching Program.)
The process of increasing the physician supply takes time, and is complicated by multiple hurdles. Most advocates agree that the first step is to expand the number of medical school students, both by increasing enrollments at existing schools and creating new ones.
In 2006, the AAMC set a goal of increasing medical school enrollment by 30 percent by 2015. Enrollments at existing schools have expanded modestly, and, in recent years, nearly two-dozen new medical schools have opened or are in the process of being accredited. (It generally take years for these schools to begin operating at full capacity, however. Even then, it is likely that, in the aggregate, they will only graduate several hundred more students each year.)
The result of these efforts so far has been relatively small increase in enrollment — from 2006 to 2010 the number of students enrolling in U.S. medical schools increased by 7.5 percent.
But that increase — or a greater one — won’t necessarily translate into more doctors. In order to become practicing physicians, graduates must complete at least three years of residency training, usually in large teaching hospitals. Without more residency slots, the number of physicians entering the workforce cannot increase. (If the number of U.S. medical school graduates increased, but the cap were left in place, graduates of U.S. medical schools, who have preference for residency slots, would replace graduates of foreign schools, but that would have no net impact on total physician supply.)
Logjam in residencies
The logjam in residency openings stems from the 1997 Balanced Budget Act. At that time, the number of residency slots funded by Medicare (the principal source of residency funding) was capped at around 100,000, and that cap has remained in place ever since.
Since the cap was set in 1997, there has been a slight increase in the total number of residency positions. Experts say, however, that most of these new positions — which are usually funded directly by the teaching hospital — are not first-year residencies, and cater instead to advanced training in specialty medicine.
Michael Whitcomb, who has served as the dean of a number of medical schools and has also worked for the AMA and the AAMC, said that “the determinate factor of physician supply in this country is the number of entry-level positions in the country’s graduate education system.”
But George Sheldon identified another obstacle. Even if the number of residency positions funded through Medicare were increased tomorrow, he said, the current infrastructure at teaching hospitals wouldn’t be able to handle a large number of new residents.