Recruitment of foreign physicians: a zero-sum equation?
Additionally, residency programs in many states, such as New York, already have recruitment in place programs to attract foreign medical graduates. Those programs could theoretically serve as models for hospitals and health centers that want to employ foreign physicians who have already completed residency training abroad.
Salsberg, who is opposed to relying more heavily on foreign doctors, said that he didn’t see recruitment being part of U.S. policy anytime soon.
“We haven’t even gotten to the point where we’re accrediting foreign medical schools yet,” he said. Last year, the Educational Commission for Foreign Medical Graduates (ECFMG) announced that it will be 2023 before it requires all foreign physicians to graduate from a medical school that has been accredited by the Liaison Committee on Medical Education.
Passive recruitment
Much of the effort to increase the U.S. physician supply has centered on increasing the number of medical residency positions — or graduate medical education (GME) slots — that are partially funded by the government, primarily through Medicare. The number was capped at about 100,000 in 1997.
The Association of American Medical Colleges and the American Medical Association argue that the U.S. will not be able to meet its need for more physicians if the cap remains in place.
But if the cap were lifted immediately, residency programs would not find large numbers of U.S. medical school graduates ready to fill newly-created spots. Nearly all graduates of domestic medical schools are already “matched” into residency programs. Thus, unless U.S. medical school enrollments were greatly expanded — as many have urged, so far unsuccessfully — an increase in the residency cap would effectively result in residency programs turning to IMGs to fill most of the new slots.
Historically, some justification for limiting U.S. reliance on foreign medical graduates has been based on questioning the quality of those graduates.
Elizabeth Garvish, an immigration attorney based in Atlanta, argued that foreign medical graduates provide at least the same level of care as U.S. trained physicians, and already have to pass several tests before they can even apply to a U.S. residency program. Those tests include an examination of clinical knowledge, a hands-on clinical skills exam, and an English-language exam.
A study by researchers at the Foundation for Advancement of International Medical Education and Research, published last year, reinforced that argument. The study found that foreign graduates perform as well as U.S. graduates, and actually perform better than American nationals who attended medical school abroad and then return to do their residency training in the U.S.
Currently, there is a high level of competition for IMGs who seek a residency slot in the U.S. Though 93 percent of U.S. medical school graduates were matched last year to first-year residency positions in the U.S., only 40 percent of IMGs were. What would happen if significantly more residency positions were created and then filled by IMGs?
Salsberg acknowledged that there would be a short-term reduction in the competitiveness of U.S. residency slots for graduates of foreign medical schools if the cap on residencies were lifted in the near future, and added: “That’s just another reason why we have to get our production up domestically.”
Brain Drain
Even if the quality of foreign physicians were ensured, Kate Tulenko, director of Intrahealth, a public health organization, argued that, when viewed internationally, physician migration is inherently a zero-sum equation.
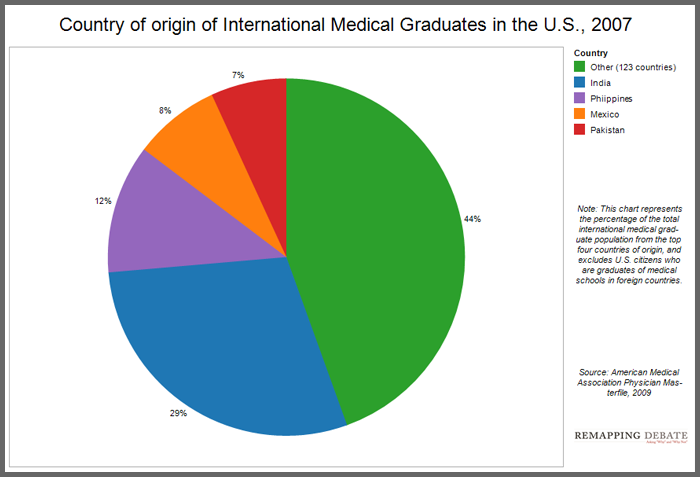
After U.S. nationals who travel abroad to attend medical school (who are still considered international medical graduates), the largest numbers of IMGs come from India, the Philippines, Pakistan, and Mexico (see chart below). Tulenko pointed out that all of these countries have physician shortages of their own, and that the World Health Organization has classified India and Pakistan as “health workforce crisis countries.”
Many of the foreign physicians who would be recruited to work in the U.S. would likely come from these same countries, Tulenko said.
“The countries that people come from are left without healthcare workers to take care of their pressing needs,” she said, adding that recruitment of physicians by wealthy countries and recruitment of nurses by the U.S. have only exacerbated the problem.
Bourgeault agreed, calling reliance on foreign physicians an “ethical gray area.” The policy of recruiting nurses from abroad has also been widely critiqued on brain drain grounds. Indeed, Salsberg pointed out that last year, the U.S. signed a “code of practice,” along with 193 other countries at the World Health Assembly, in which voluntary principles for “the ethical international recruitment of health personnel” were endorsed in order to lessen recruitment from lower income countries with “fragile health systems.”
Garvish dismissed ethics-based arguments against foreign recruitment, saying that it “may be the case” that the U.S. is depriving other countries of their health workforce, “but I don’t know if the U.S. is supposed to make sure that every country out there has enough qualified doctors to care for their people. It’s a free world, and I think the U.S. needs to deal with its own issues.”
Tulenko, however, argued that the reliance on foreign medical graduates is so unethical that the U.S. should dramatically increase medical school enrollments before adding any new residency positions.
Cooper acknowledged that, because of these ethical issues, foreign recruitment of physicians would not be a good long-term strategy, and should only be employed in the short-term as the U.S. simultaneously ramps up its education and training capacity.